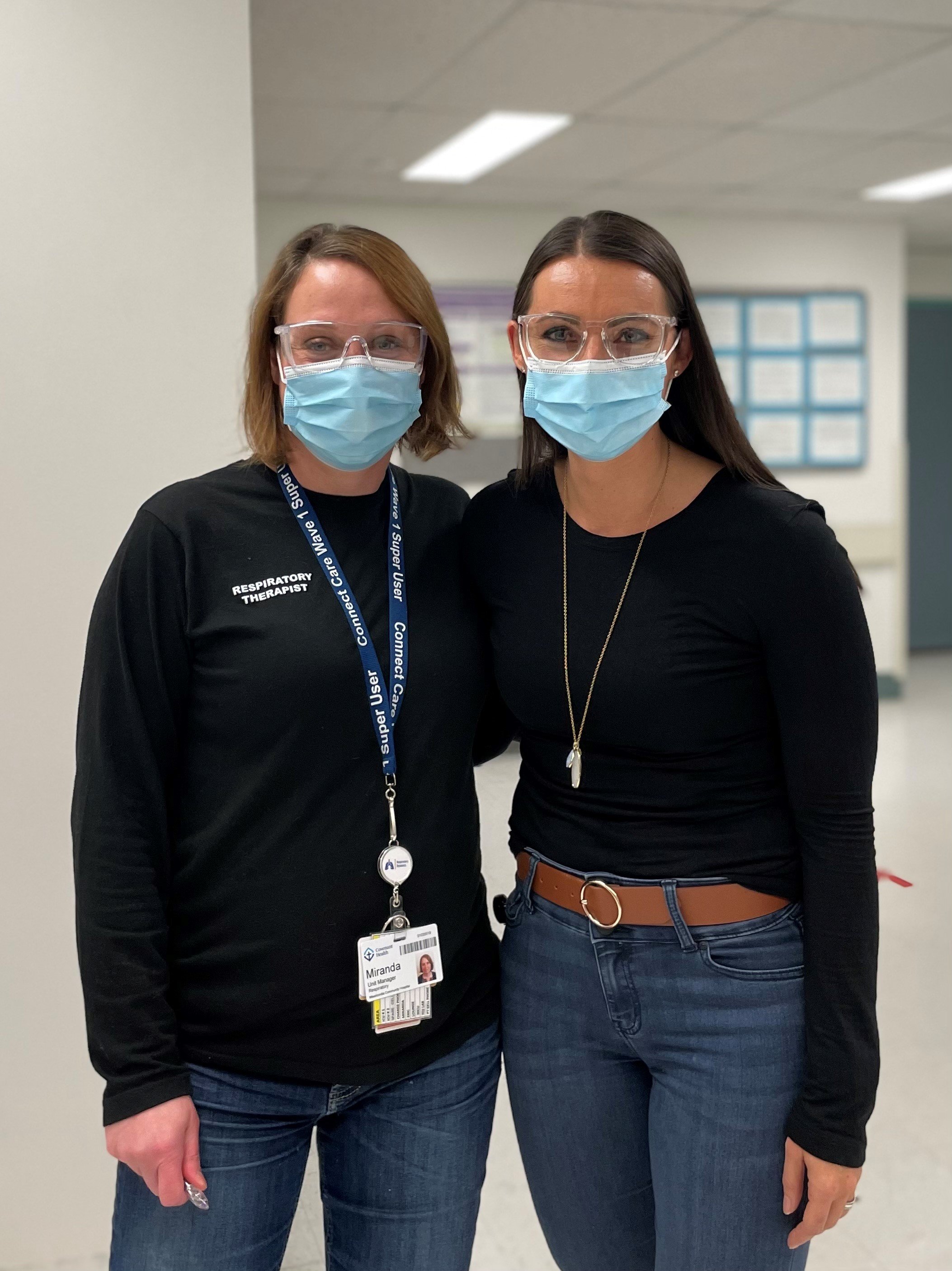
Rehabilitation medicine and respiratory therapy
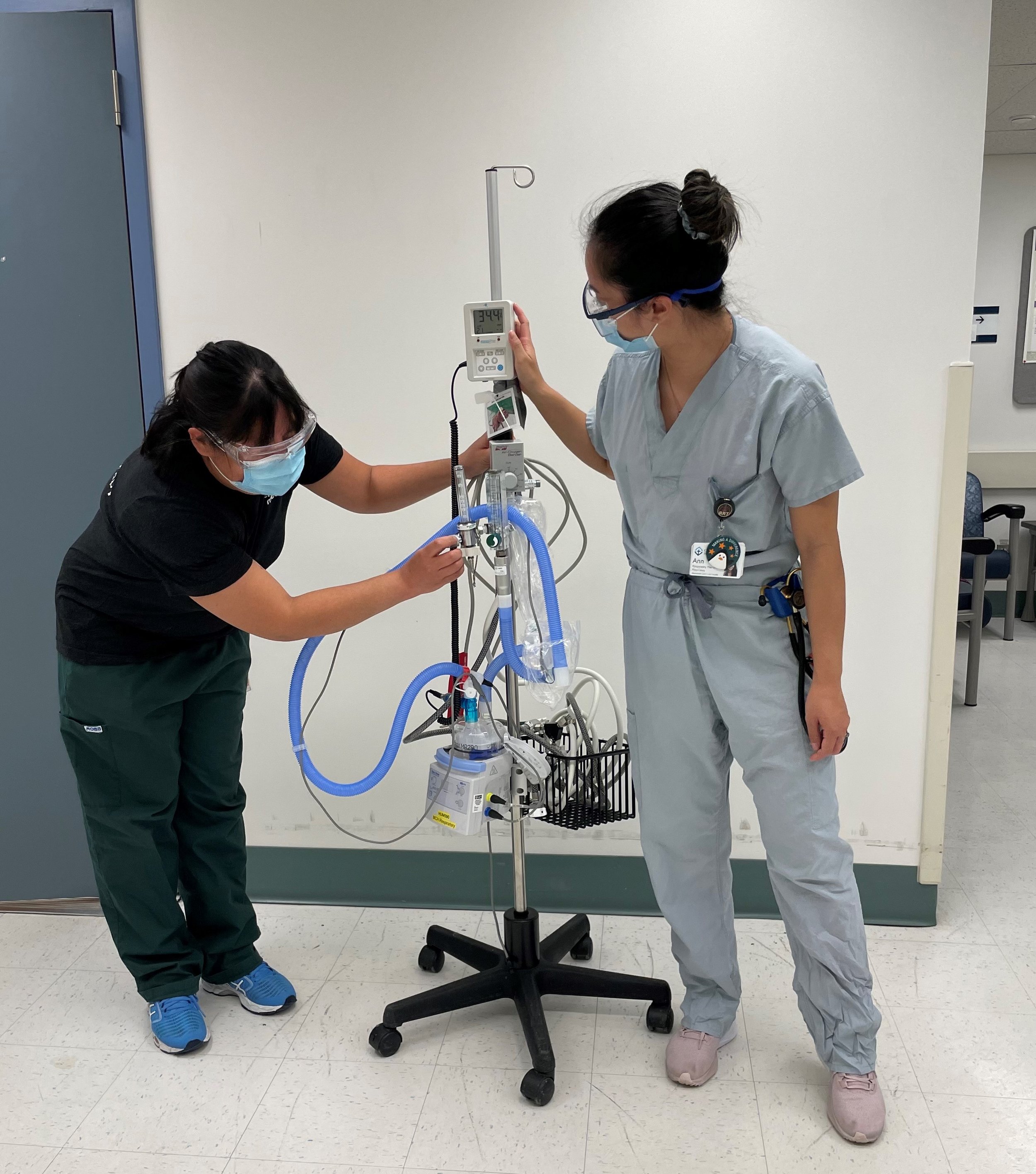
The COVID-19 pandemic led to an unprecedented increase in hospitalized patients requiring oxygen management and cardiopulmonary treatments, with a 300 per cent increase in patients at Misericordia Community Hospital (MCH) requiring heated humidified high flow oxygen (HHHFO) by the fourth wave. Patient care service specific to oxygen management falls within the role of registered respiratory therapists (RRTs) at the MCH. Physical therapists (PTs) are trained to carry out oxygen therapy, but did not perform this role at MCH. With increasing patient care pressures due to the COVID-19 pandemic, it was identified that PT could be a key resource to assist the respiratory therapy (RT) department.
In collaboration with professional practice, PT and RT quickly developed a comprehensive orientation plan during both Waves 2 and 4. They created education materials and training guidelines for PTs to be able to take on this "out of the box" role supporting RRTs to provide care for patients with cardiopulmonary and oxygen management needs. They also identified additional resources that rehabilitation could provide to the RT department and determined that therapy assistants (TAs) could alleviate some work load from the RRTs by completing their daily inventory and oxygen cylinder re-stocking throughout the hospital.
The support from PT and TAs allowed RRTs to focus on caring for patients with increasing demands for complex and/or critical oxygen needs. RRTs were able to maintain the same quality of care for patients despite the increased demands. The rehabilitation and respiratory therapy departments demonstrated exceptional stewardship by working within existing resources to evolve and meet the unprecedented demands of COVID-19 on the healthcare system. The staffing support that was provided by the rehabilitation department led to less RRT overtime to achieve their baseline staffing (and decreased the overall magnitude of RRT burnout). PT staff were able to serve 150 RT patients over eight weeks, spanning multiple periods of reassignment, all while continuing to meet their own professional inpatient rehabilitation activity targets.
The reassignment model of care used at MCH was also spread and scaled to small urban and rural sites within the province. St. Mary’s Hospital in Camrose was able to leverage this model to support a respiratory hub to address the surge in respiratory care needs for patients in their surrounding communities.